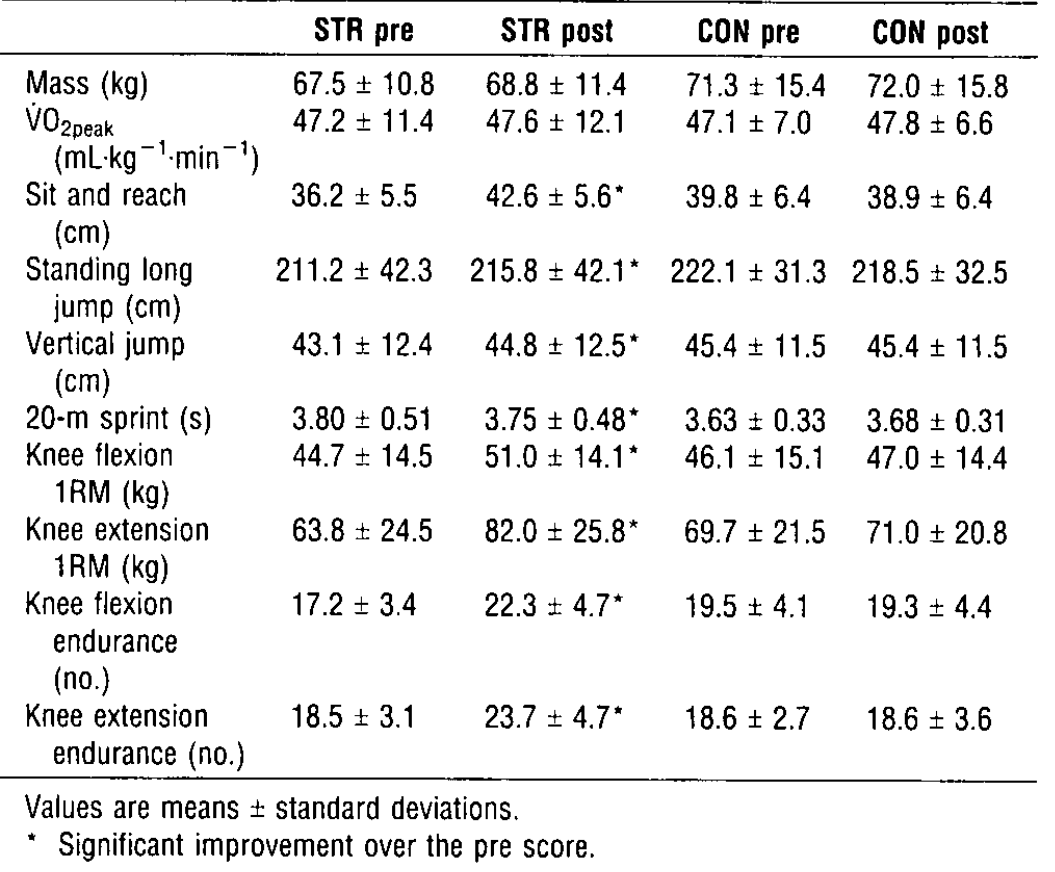
Sports injuries are a major roadblock for athletes, keeping them from playing their best, or even at all. Even after an injury is healed, athletes have to build back up muscles that atrophied over recovery time. During rehab time, patients undergo different exercise routines to build the muscle that was left unused while the injury was healing. But how do the trainers know when it is safe to allow the athlete back in the field?
One way to quantify the “readiness” of the player is by using an Isokinetic Dynamometer machine to determine how much power the questioned muscle can exert and how that compares to its counterpart. For example, let’s say a female athlete tears her right ACL. Throughout her rehabilitation, her trainers will set her up on an Isokinetic Dynamometer machine (Figure 1) to determine the power exerted by the right quadricep and hamstring, which are muscles that commonly experience atrophy during ACL recovery, and compare it to the power of her left quadricep and hamstring. Based on the presettings of range of motion, force, and speed, the device can calculate the torque provided by the athlete and then multiply it by the constant speed (isokinetic part) to find the power exerted by those specific muscles. It is obvious that time is needed to heal, but every patient is unique and time could vary. It is important to find a quantitative way to determine when each patient is back to normal strength and this design does just that.
One patent of an isokinetic dynamometer is the “Exercise Physical Rehabilitation and Testing Method and Apparatus” (Patent number: 5,722,937), which was filed in April 17, 1996 and issued on March 3, 1998. Invented by James F. Smith, it is still used by assignee Cybex International, Inc to this day. U.S. classifications are as followed: 601/23; 601/24; 482/4; 482/137; 482/142; 482/908.

Figure 1: Set-up of limb to lever arm and dynamometer. The user pushes leg up and back and the dynamometer, comprised of the motor and cycloidal speed reducer, monitors and alerts the computer if the motor needs to slow down or speed up to keep a constant speed depending on the torque exerted by the user.
The main claims of a total 30 for this patent is to help athletes and patients in rehabilitation for muscle atrophy or decreased muscle strength by evaluating the strength of a targeted muscle by forcing the patient to keep a constant speed through resistance. This machine consists of a base with a track to allow adjustability of the chair to customize the fit for each user. There is also a lever arm, where the user will push against during exercises, connected to the chair and to the dynamometer. The dynamometer is comprised of a motor to change torque and a cycloidal speed reducer with a high and low speed shaft to keep a constant speed during exercise (Figure 1). This machine helps build muscle fibers by forcing the patient/athlete to provide maximum force to move a lever arm while the machine provides resistance (or takes away) to keep the patient moving at a constant speed. Not only can this machine provide biofeedback on the power of the muscle to help physical therapists plan an exercise regimen to help patients, but it can also help athletes build their muscles and ensure their body is balanced to avoid straining and injury. This device has various protocols that subjects the muscles of the user to “concentric or eccentric motion in isotonic or isokinetic modes or continuous passive motion.”
Physical Therapists, Athletic Trainers and athletes will primarily use this machine. It is very bulky and expensive, so only established facilities can afford this technology. This product helps physical therapists and athletic trainers assess the muscle strength of their patients to determine what the state of the targeted muscle strength is and help them prepare an exercise routine to get their patients to where they need to be to be healthy and avoid further injury. Athletes can also use this technology to grow muscles due to the max force and full range of motion the lever and program provide. This product is designed for determining when muscles have developed enough to start playing again after suffering from atrophy during rehabilitation.

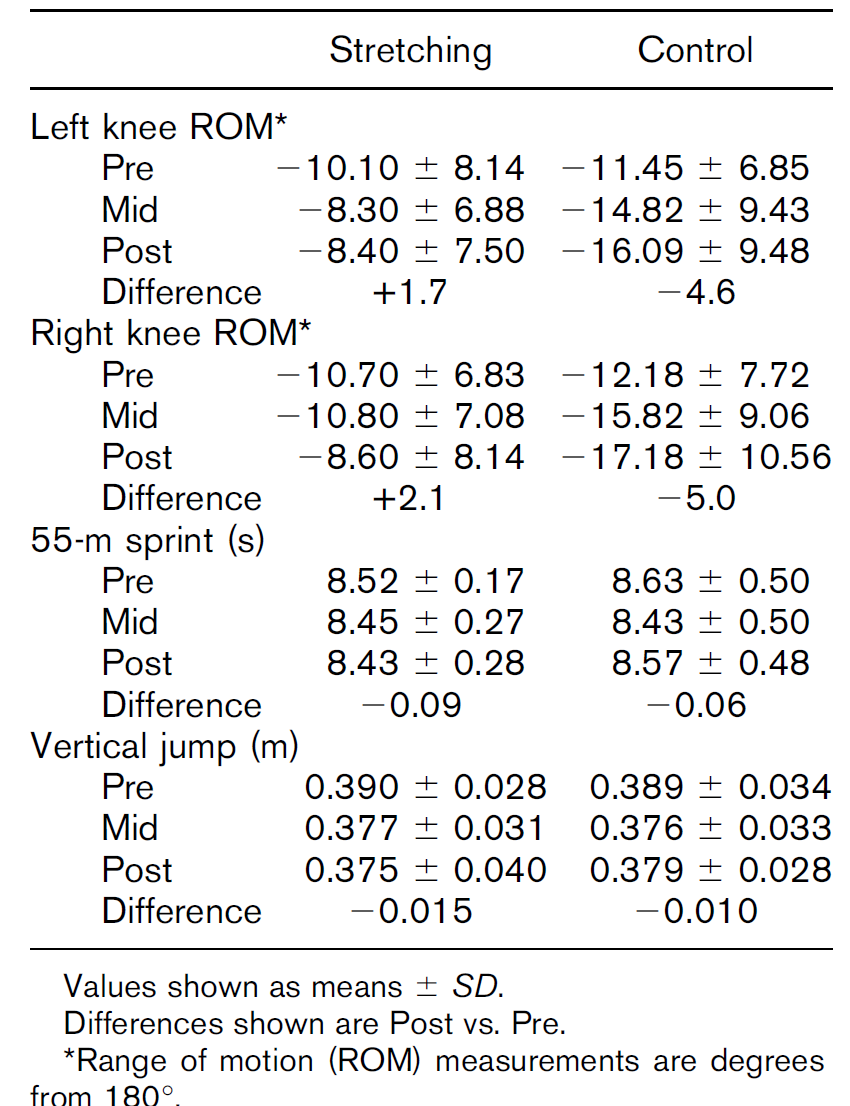
Figure 2: Schematic of Isokinetic Concentric mode feedback loop depending on the performance of the user. If threshold torque is too high, the motor will accelerate. If threshold torque is too low, motor will decelerate to zero speed.
Patients sit in an upright position and strapped at the waist and thigh to stabilize the body and to force the patient to only use the targeted muscle. Next, after setting up the machine with the desired weight and speed, the patient must push and pull a lever arm as hard as they can. The lever arm, attached to a low speed shaft of a cycloidal speed reducer follows a negative feedback and the machine. For example, Isokinetic Concentric mode, the mode most commonly used for determining the power produced by the muscle, uses the dynamometer control board to determine the angle (boundaries of range of motion) of the lever arm and signals the dynamometer to slow down to a stop until the user pushes the lever arm in the other direction. The torque on the dynamometer control board, which is measured by strain gauges, is sampled every two milliseconds. The computer monitors the the measured torque (force of the limb attached to the lever arm multiplied by the distance to the targeted muscle) and compares it to the threshold torque. If the measured is greater than the threshold, the motor will accelerate (less resistance) based on the magnitude of the torque and the direction of the measured torque to approach the isokinetic speed. If the measured torque is not sufficient, the motor will decelerate to zero speed until sufficient torque is met (Figure 2).
Compared to other designs, this patent is less costly, smaller in size, and has less parts. Also, the speed reducer incorporated in this design does not create a high pitch noise that is disruptive in quiet clinical scenes, which was commonly found in previous designs. As for the infrastructure of the machine, this new design fixes a previous problem of slack resistance during start up, which creates a loose and not smooth feeling for patients (also known as backlash). The slack would allow for additional bending torque on the shafts, which creates that loose and unnatural feel. This design fixes this problem because the cycloidal speed reducer specific to this design has a higher torsional stiffness. The cycloidal speed reduces also has a longer life and will reduce the overall effect of backlash throughout time. This patent is still the primary patent for CSMi Medical Solution’s HumacNorm Testing and Rehabilitation System, so it is reasonable to assume these claims are valid and the design is reliable and effective!
Source:
Smith, J.F. (1998). U.S. Patent No. 5,722,937. Retrieved from http://pdfpiw.uspto.gov/.piw?PageNum=0&docid=05722937&IDKey=C45CA52352DA%0D%0A&HomeUrl=http%3A%2F%2Fpatft.uspto.gov%2Fnetacgi%2Fnph-Parser%3FSect1%3DPTO1%2526Sect2%3DHITOFF%2526d%3DPALL%2526p%3D1%2526u%3D%25252Fnetahtml%25252FPTO%25252Fsrchnum.htm%2526r%3D1%2526f%3DG%2526l%3D50%2526s1%3D5%2C722%2C937.PN.%2526OS%3DPN%2F5%2C722%2C937%2526RS%3DPN%2F5%2C722%2C937