My first exposure to cupping was seeing the perfectly circular bruises on Michel Phelp’s during the 2016 Summer Olympics. Since then, I have come across it many times in the University of Delaware athletic training room seeing athletes performing exercises with cups suctioned to their back. I have even tried it myself a couple of times to see what the hype was about and if I felt a difference using this type of recovery method.
Figure 1. Michael Phelps swimming with visible cupping markers (bruises) on his shoulders.
Now if you haven’t heard about cupping you may be wondering: what is cupping? Cupping is the application of plastic, glass, bamboo, or ceramics cups [1] to the skin via suction. The suction can either be created naturally by heating up the inside of the cup using a flame and allowing it to cool on the skin creating negative pressure and lifting/stretching the skin up. The other way to get this pressure is to use a suction device.[1] There are also two types of cupping, similar to needling; there are both wet and dry methods. Dry cupping is exactly the procedure I described above while wet cupping is when small cuts are made on the skin before the cup is applied and blood is drawn out. [1] The original idea behind this technique was that it was regulating Qi in the body. More recently, people claim that it promotes blood flow and therefore has a positive effect on the healing process, reducing soreness and pain. There are still many who find cupping bizarre and disgusting due to the often dark bruising and the odd look of the skin suctioned into cups. In particular, a Forbes article by Steven Salzberg goes as describes it as “someone giving you a massive hickey, and then doing another dozen or so all over your back, or legs, or wherever ” [2]. So by now, you should have a pretty clear image that while there are many advocates and cupping has been gaining interest (especially if professional athletes on the world stage have used it), there are still many skeptics and people who say it is harmful. Let’s see exactly what the research says about cupping. Is it beneficial? Harmful?
An article published in The Journal of Alternative and Complementary Medicine by a group of Australian and German researchers performed a systematic meta-analysis of clinical trials evaluating the effects of cupping on athletes. [3] They found 11 valid (according to their criteria) trials with a combined total of 498 participants from China, the United States, Greece, Iran, and the United Arab Emirates. Participants received cupping 1 to 20 times in daily or weekly intervals either alone or in combination with another procedure, like acupuncture.[3] The study found no conclusive results however. Even though there were improvements to the participant’s perception of pain, an increased range of motion, and lower levels of creatine kinase, there were large variations between symptom intensity and recovery measures, and other metrics.[3] There are also some limitations to this study. One of the main concerns is the reliability of the data. The researchers report an unclear or high risk of bias in many of the trials and they also mention that none of the trials reported safety.
Another study published in 2016 in the Journal of Novel Physiotherapies evaluated the effects of various soft tissue mobilization techniques, including cupping, on active myofascial trigger-points in 20 amateur soccer players.[4] Athletes received cupping once a week for three weeks. They found that all techniques used, including cupping, improved pain pressure threshold and pain sensitivity significantly. [4] The researchers concluded that more research must be done to fully be able to draw a conclusion. Some limitations of the study were the small sample size (n = 20) and that the study was limited to only amateur soccer players. Other studies, including the previously mentioned study viewed multiple different sports instead of one. This also provided a much larger sample size compared to this study.
Overall, there appears to be no definite answer, at least at this time, on if cupping helps promote healing and reduce pain and muscle soreness. For some, it appears to be beneficial in relieving pain but due to a limited number of studies and the questionable accuracy of others, there is no conclusive data for or against cupping. As the first-mentioned study by Bridgett et. al stated, “ No explicit recommendation for or against the use of cupping for athletes can be made. More studies are necessary for conclusive judgment on the efficacy and safety of cupping in athletes.” [3].
References:
[1] NCCIH. “Cupping.” November 2018. Retrieved from: https://www.nccih.nih.gov/health/cupping
[2] Steven Salzberg. “ The Ridiculous and Possibly Harmful Practice of Cupping”. May 2019. Retrieved from: https://www.forbes.com/sites/stevensalzberg/2019/05/13/the-ridiculous-and-possibly-harmful-practice-of-cupping/#57ce2d2331f3
[3] Rhianna Bridgett, Petra Klose, Rob Duffield, Suni Mydock, and Romy Lauche.The Journal of Alternative and Complementary Medicine.Mar 2018. 208-219.http://doi.org/10.1089/acm.2017.0191
[4] Fousekis, Konstantinos et al. “The Effectiveness of Instrument-assisted Soft Tissue Mobilization Technique(Ergoné Technique), Cupping and Ischaemic Pressure Techniques in the Treatment of Amateur AthletesàMyofascial Trigger Points.” (2016).
Questions to Consider:
- Have you ever gotten cupping done? If yes, what are your thoughts? Did you find it beneficial? If no, was there a reason why?
- How do you think studies looking at cupping should compare its effects for the most accurate evaluation? Should they compare across different sports because the benefits should not be sport dependent or within one sport to get a better comparison?



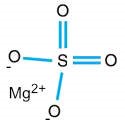
 I did however find articles about other medical uses for magnesium sulfate. In the study from Maternal-Fetal Medicine Units Network, they wanted to test if magnesium sulfate could help prevent cerebral palsy in preterm babies. 2241 women at imminent risk for delivery between 24 and 31 weeks of gestation, were randomized into experimental (magnesium sulfate) and placebo (control) groups. Each group receive magnesium sulfate, administered intravenously as a 6-g bolus followed by a constant infusion of 2 g per hour, or matching placebo. After a follow up analysis, the rate of the primary outcome was not significantly different in the magnesium sulfate group and the placebo group. However, in a secondary analysis, moderate or severe cerebral palsy occurred significantly less frequently in the magnesium sulfate group. The risk of death did not differ significantly between the groups.
I did however find articles about other medical uses for magnesium sulfate. In the study from Maternal-Fetal Medicine Units Network, they wanted to test if magnesium sulfate could help prevent cerebral palsy in preterm babies. 2241 women at imminent risk for delivery between 24 and 31 weeks of gestation, were randomized into experimental (magnesium sulfate) and placebo (control) groups. Each group receive magnesium sulfate, administered intravenously as a 6-g bolus followed by a constant infusion of 2 g per hour, or matching placebo. After a follow up analysis, the rate of the primary outcome was not significantly different in the magnesium sulfate group and the placebo group. However, in a secondary analysis, moderate or severe cerebral palsy occurred significantly less frequently in the magnesium sulfate group. The risk of death did not differ significantly between the groups.