Wrist pedometers are used by many to count their steps, and notify users when they “reach their 10,000”. These wearable devices quantify step activity and give indiviudals an idea of exactly how much they are moving throughout the day.
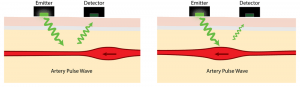
Accelerometers are often used within these wearable devices to detect the force acting on the device. The force acting on the accelerometer is correlated to an analog voltage output, which must be processed through a series of op amps to turn a users movement into an electrical output that can be analyzed through signal processing, but what signal processing circuitry is needed following the accelerometer within a wrist pedometer to correlate force acting on the pedometer to steps taken by the user?
In this post we will solve at the following engineering problem associated with pedometers: what signal processing circuitry is needed to convert the analog voltage input from an accelerometer to a binary digital signal that can be correlated to steps taken by a user?
Background
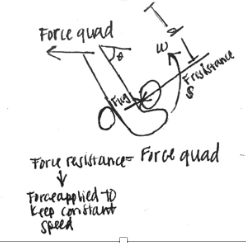
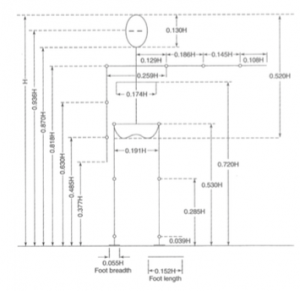
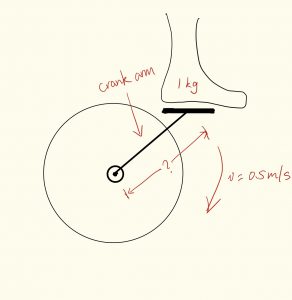
The average person takes between 0 and 120 steps per a minute. Throughout each gait cycle, a wrist pedometer experiences forces relative to its position, as shown in Figure 1. While standing the force detected by the pedometer is 1G (one times the force of gravity). When a user is pushing against the ground to step forward the force detected by the pedometer can rise above 1G, and while the user is between steps the force detected by the pedometer can go below 1G. The pedometer can detect when a user takes a step by monitoring forces and determining when the 1G threshold is crossed. Many wrist pedometers use a threshold of at least +/- 0.2G to prevent noise and standing movements from being accounted for in step count. So a step count will be equal to crossing the 1.2G and -1.2G thresholds[1].Accelerometers are often used to relate the force acting on an object to an electrical signal. Analog Devices, a circuitry component manufacturer, produces an +/- 2g accelerometer that relates forces between -2g and +2g to a voltage output, as shown in Figure 2. A linear region exists between +/- 2g, which can be defined by the following simplified function V(g)=(.875*g)+2.5 [2].
Approach
In designing the signal processing circuitry necessary to convert an analog signal from an accelerometer to a binary digital signal, we will do the following:
1.Define the input signal in terms of force acting on a wrist pedometer, and the voltage output of an accelerometer
2.Determine the signal processing necessary to convert the analog signal into binary digital output
3.Select circuit components to complete desired signal processing, and appropriate values for integrated components
4.Use LTSpice to model desired circuitry, and confirm that designed circuit solves the defined engineering problem
Signal Input
It is known that the force acting on a wrist pedometer can be defined by a sine wave function fluctuating +/ 0.5g around 1g, with a frequency of 0-2Hz. Therefore we will define the force acting on the pedometer as F(t)= 0.5sin(t) + 1g. Given the voltage output of analog devices accelerometer is V(g)=(.875*g)+2.5, the voltage output of the accelerometer can be defined as V(t)=0.4105sin(t)+3.375.
Signal Processing
To generate a digital binary signal from an analog voltage input signal processing through circuitry is required.

Figure 5. Flow chart of signal processing of input analog signal from accelerometer to binary output signal
First, the input signal should be passed through a low pass filter, with a cutoff frequency of 2Hz to remove high frequency noise from the signal. The force acting on the pedometer, and voltage output of an accelerometer can be defined by sine wave functions. The baseline of accelerometer voltage output exists above zero volts, therefore a subtractor should be used to bring the baseline of this signal to 0V. A full wave rectifier will be used as an AC to DC converter, converting both polarities of the signal to a pulsating DC signal. A compactor will be used to produce a binary DC output that indicates whether the signal is above a given threshold, voltage relative to passing +/- 0.2g force threshold. This binary signal is the system output and can be used to count total steps taken by a user.
Circuit Components
Circuit components were selected to complete necessary signal processing, and assumed to be ideal for simplification of solving this problem.
Low pass filter
With a cutoff frequency of 2Hz, a low pass filter with a Capacitor of 4.7 nF and resistor of 0.0169 Ohms can be used to filter out high frequency noise
Follower
Follower used to preserve signal and prevent current flow back to the user
Subtractor
A subtractor can be used to reduce the baseline signal to zero. Given our voltage input is V(t)=0.4105sin(t)+3.375 V, and the Voltage output of this component is Vout = (R3/R1)*(Vin-Vs), we will set Vs=3.375V DC and R1=R2=R3=100 Ohm to bring the baseline signal down to 0V.
Full Wave Rectifier
A full wave rectifier will be used to convert all polarities of the input signal to the same polarities. If R1=R2=R3=R4=R5, then if Vin>0 Vout=Vin and Vin<0 Vout=-Vin. Therefore, we will set all the resistors equal to each other to achieve a rectified DC signal.
Comparator
A comparator will be used to convert the pulsating DC signal to a binary digital output. Op amps functioning as comparators follow the rule that if V+>V- Vout = Vc+ and V->V+ Vout=Vc-. In our ideal circuit, we aim our binary signal to be either 0 or 1.
V+ terminal will be our signal, and we look to determine if this signal represents crossing the 1.2g threshold. To find what the V- terminal should be we need to determine the voltage at this point in the circuit if it has crossed the threshold. Given, V(g)=(.875*g)+2.5, V(g=1.2)=3.52. The signal is brought through a subtractor where it is reduced by 3.375 and afterword is no longer amplified or modified, so the threshold voltage at this point is 0.1534 V. The negative input terminal will be set to be a DC voltage of 0.1534V.
To generate a binary output where 0V= not crossing the threshold and 1V= crossing threshold, the op amp terminals will be set to be Vc+ = 1V and Vc-=0V.
LTSpice Modeling and Verification

Figure 11. LTSpice signal processing circuit following accelerometer to convert analog accelerometer signal input to binary output
LTSpice was used to model the designed circuit, as shown in figure 11. This circuit was simulated using LTSpice software and it’s ability to produce a binary digital output from an analog signal was verified as depicted in figure 12.
Solution
Our goal was to design signal processing circuitry is needed to convert the analog voltage input from an accelerometer to a binary digital signal that can be correlated to steps taken by a user.

Figure 13. Accelerometer analog output signaling processing circuit to produce binary digital output
A series of signal processing components were integrated within a circuit, depicted in figure 13, to convert an analog voltage signal from an accelerometer into a binary digital signal. This circuit removes high frequency signal noise, reduces the signal baseline, generates a pulsating DC signal, and generates a binary signal output, as shown in figure 14.
This binary digital output can be correlated to steps taken, as two square waves is equal to one step taken. These square waves can be counted by an integrated software and used to count user steps. Thus, turning the analog accelerometer voltage output into a binary digital signal.
This binary signal can be used to count steps and step frequency, and when integrated with GPS and other technologies can be used to determine step distance and user speed.
With one two sqaure waves equaling a step, the designed integrated circuit turns user movement into step count, enabling the signal processing necessary to count those 10,000 steps everyone is so desperately trying to reach!
References
[1] Modi, Yash Rohit. (2014). United States Patent No. US20140074431A1. Retrieved from https://patents.google.com/patent/US20140074431A1/en
[2] “Accelerometer Specifications – Quick Definitions.” Accelerometer Specifications – Quick Definitions | Analog Devices, www.analog.com/en/products/landing-pages/001/accelerometer-specifications-definitions.html.